Notes on Glomerular Filtration Rate (GFR) – Renal Physiology, MCQ with answer and Lecture
admin GPAT Lectures, Human Anatomy And Physiology, MCQ, NEET Biology, NEET PG, NEET UG Chart Factors Affecting GFR, Clinical Relevance of GFR, Factors Affecting GFR, MCQ on Glomerular Filtration Rate (GFR), MCQ on Renal Physiology, MCQ on Urinary System with Answer, MCQ on Urinary System with Answer for GPAT, MCQ on Urinary System with Answer for NEET, Renal Physiology Related to GFR, Starling Forces Affecting GFR, What is GFR?
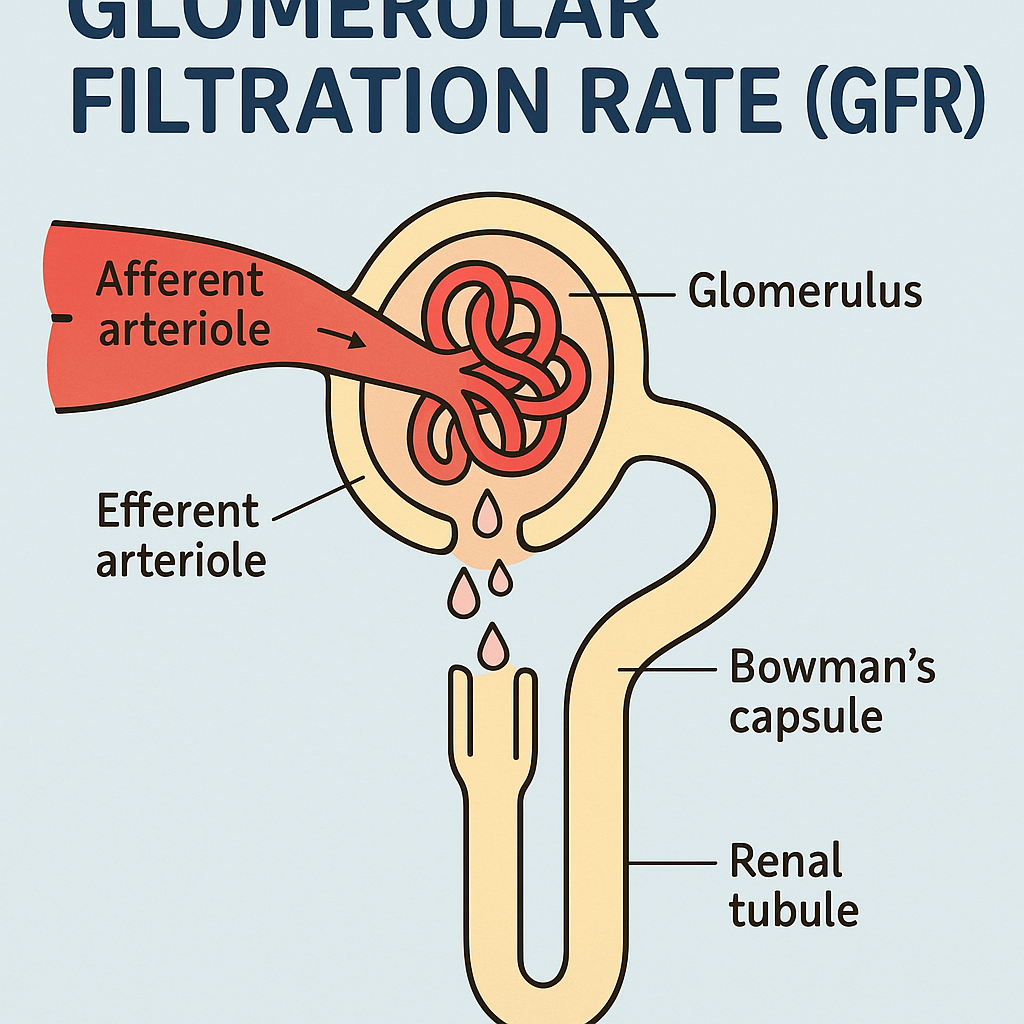
What is GFR?
- Definition: Glomerular Filtration Rate (GFR) is the volume of fluid filtered from the glomerular capillaries into the Bowman’s capsule per unit of time. It measures kidney function and filtration efficiency.
- Normal Value: Approximately 125 mL/min in healthy adults (180 L/day), though it varies with age, sex, and body size.
- Purpose: GFR reflects the kidneys’ ability to filter blood and remove waste while retaining essential substances.
Get full Lecture Series of Urinary System: Click Here
Renal Physiology Related to GFR
- Glomerulus: A network of capillaries in the nephron where filtration occurs.
- Bowman’s Capsule: Collects the filtrate from the glomerulus.
- Filtration Membrane: Composed of three layers:
- Fenestrated Endothelium: Allows passage of water, ions, and small molecules; restricts large proteins and cells.
- Basement Membrane: Acts as a selective barrier, preventing filtration of proteins like albumin.
- Podocytes: Specialized cells with filtration slits that fine-tune filtration.
- Filtration Process: Driven by Starling forces (hydrostatic and oncotic pressures).
Starling Forces Affecting GFR
- Net Filtration Pressure (NFP) = GFR driving force:
- Glomerular Hydrostatic Pressure (P_GC): ~60 mmHg (pushes fluid out of capillaries).
- Bowman’s Capsule Hydrostatic Pressure (P_BC): ~15 mmHg (opposes filtration).
- Glomerular Oncotic Pressure (π_GC): ~25 mmHg (opposes filtration due to plasma proteins).
- Formula: NFP = P_GC – (P_BC + π_GC) ≈ 10 mmHg.
Factors Affecting GFR
- Blood Pressure:
- Increased systemic BP increases P_GC → ↑ GFR.
- Decreased BP (e.g., hemorrhage) → ↓ GFR.
- Afferent Arteriolar Resistance:
- Constriction (e.g., sympathetic activation) → ↓ GFR.
- Dilation → ↑ GFR.
- Efferent Arteriolar Resistance:
- Constriction (e.g., angiotensin II) → ↑ P_GC → ↑ GFR (up to a point).
- Dilation → ↓ GFR.
- Plasma Protein Concentration:
- Hypoproteinemia (↓ π_GC) → ↑ GFR.
- Hyperproteinemia → ↓ GFR.
- Bowman’s Capsule Pressure:
- Obstruction (e.g., kidney stones) → ↑ P_BC → ↓ GFR.
- Renal Blood Flow (RBF):
- Directly proportional to GFR; reduced RBF (e.g., dehydration) → ↓ GFR.
- Autoregulation:
- Maintains stable GFR despite BP changes (via myogenic mechanism and tubuloglomerular feedback).
- Effective between 80-180 mmHg mean arterial pressure.
- Hormonal Regulation:
- Angiotensin II: Constricts efferent arteriole → ↑ GFR.
- ANP (Atrial Natriuretic Peptide): Dilates afferent arteriole → ↑ GFR.
- Sympathetic NS: Constricts afferent arteriole → ↓ GFR.
Clinical Relevance
- GFR Estimation: Measured via creatinine clearance or estimated using equations (e.g., Cockcroft-Gault, MDRD).
- Decreased GFR: Indicates kidney damage (e.g., chronic kidney disease).
- Increased GFR: Seen in early diabetes (hyperfiltration).
Chart: Factors Affecting GFR
| Factor | Effect on GFR | Mechanism | Example Condition |
|---|---|---|---|
| ↑ Glomerular Hydrostatic Pressure | Increases GFR | More fluid pushed into Bowman’s capsule | Hypertension |
| ↓ Afferent Arteriolar Resistance | Increases GFR | More blood enters glomerulus | ANP release |
| ↑ Efferent Arteriolar Resistance | Increases GFR (moderately) | Higher pressure in glomerulus | Angiotensin II action |
| ↓ Plasma Protein Concentration | Increases GFR | Reduced oncotic pressure opposing filtration | Liver disease (hypoalbuminemia) |
| ↑ Bowman’s Capsule Pressure | Decreases GFR | Opposes filtration | Kidney stone obstruction |
| ↓ Renal Blood Flow | Decreases GFR | Less blood available for filtration | Dehydration |
| Sympathetic Activation | Decreases GFR | Constricts afferent arteriole | Stress or shock |
Multiple-Choice Questions (MCQs)
- What is the primary driving force for glomerular filtration?
- A) Bowman’s capsule hydrostatic pressure
- B) Glomerular hydrostatic pressure
- C) Plasma oncotic pressure
- D) Tubular reabsorption
- Answer: B) Glomerular hydrostatic pressure
- Which of the following would most likely decrease GFR?
- A) Dilation of the afferent arteriole
- B) Constriction of the efferent arteriole
- C) Increased Bowman’s capsule pressure
- D) Increased plasma protein concentration
- Answer: C) Increased Bowman’s capsule pressure
- A patient with severe dehydration would likely exhibit:
- A) Increased GFR due to higher renal blood flow
- B) Decreased GFR due to reduced renal blood flow
- C) No change in GFR due to autoregulation
- D) Increased GFR due to higher oncotic pressure
- Answer: B) Decreased GFR due to reduced renal blood flow
- Angiotensin II primarily affects GFR by:
- A) Dilating the afferent arteriole
- B) Constricting the efferent arteriole
- C) Increasing plasma protein concentration
- D) Reducing glomerular hydrostatic pressure
- Answer: B) Constricting the efferent arteriole
- The normal GFR in a healthy adult is closest to:
- A) 50 mL/min
- B) 125 mL/min
- C) 200 mL/min
- D) 300 mL/min
- Answer: B) 125 mL/min