Glycogen Storage Disease (GSD) Notes for NEET, GPAT, UPSC, GATE, NORCET
Overview
-
Definition: Glycogen Storage Diseases are a group of inherited metabolic disorders caused by deficiencies in enzymes involved in glycogen synthesis, degradation, or regulation.
-
Inheritance: Mostly autosomal recessive, except for GSD IX (X-linked in some cases).
-
General Symptoms: Hypoglycemia, hepatomegaly, growth retardation, muscle weakness, and metabolic imbalances depending on the type.
Participate in GPAT MOCK TEST
Classification and Key Types
-
GSD Type I (von Gierke Disease)
-
Enzyme Deficiency: Glucose-6-phosphatase.
-
Pathophysiology: Impaired conversion of glucose-6-phosphate to glucose, leading to glycogen accumulation in liver and kidneys.
-
Symptoms: Severe hypoglycemia, lactic acidosis, hyperuricemia, hyperlipidemia, hepatomegaly, kidney enlargement.
-
Treatment: Frequent meals, cornstarch therapy, avoid fasting.
-
-
GSD Type II (Pompe Disease)
-
Enzyme Deficiency: Acid alpha-glucosidase (lysosomal enzyme).
-
Pathophysiology: Glycogen accumulation in lysosomes, particularly in muscles and heart.
-
Symptoms: Muscle weakness, cardiomyopathy, respiratory failure (infantile form); limb-girdle weakness (adult form).
-
Treatment: Enzyme replacement therapy (alglucosidase alfa).
-
-
GSD Type III (Cori or Forbes Disease)
-
Enzyme Deficiency: Amylo-1,6-glucosidase (debranching enzyme).
-
Pathophysiology: Accumulation of abnormal glycogen (limit dextrin) due to inability to remove branches.
-
Symptoms: Hepatomegaly, hypoglycemia, muscle weakness, mild compared to Type I.
-
Treatment: High-protein diet, cornstarch therapy.
-
-
GSD Type V (McArdle Disease)
-
Enzyme Deficiency: Muscle phosphorylase.
-
Pathophysiology: Inability to break down glycogen in skeletal muscle.
-
Symptoms: Exercise intolerance, muscle cramps, myoglobinuria (rhabdomyolysis risk).
-
Treatment: Avoid strenuous exercise, carbohydrate intake before activity.
-
-
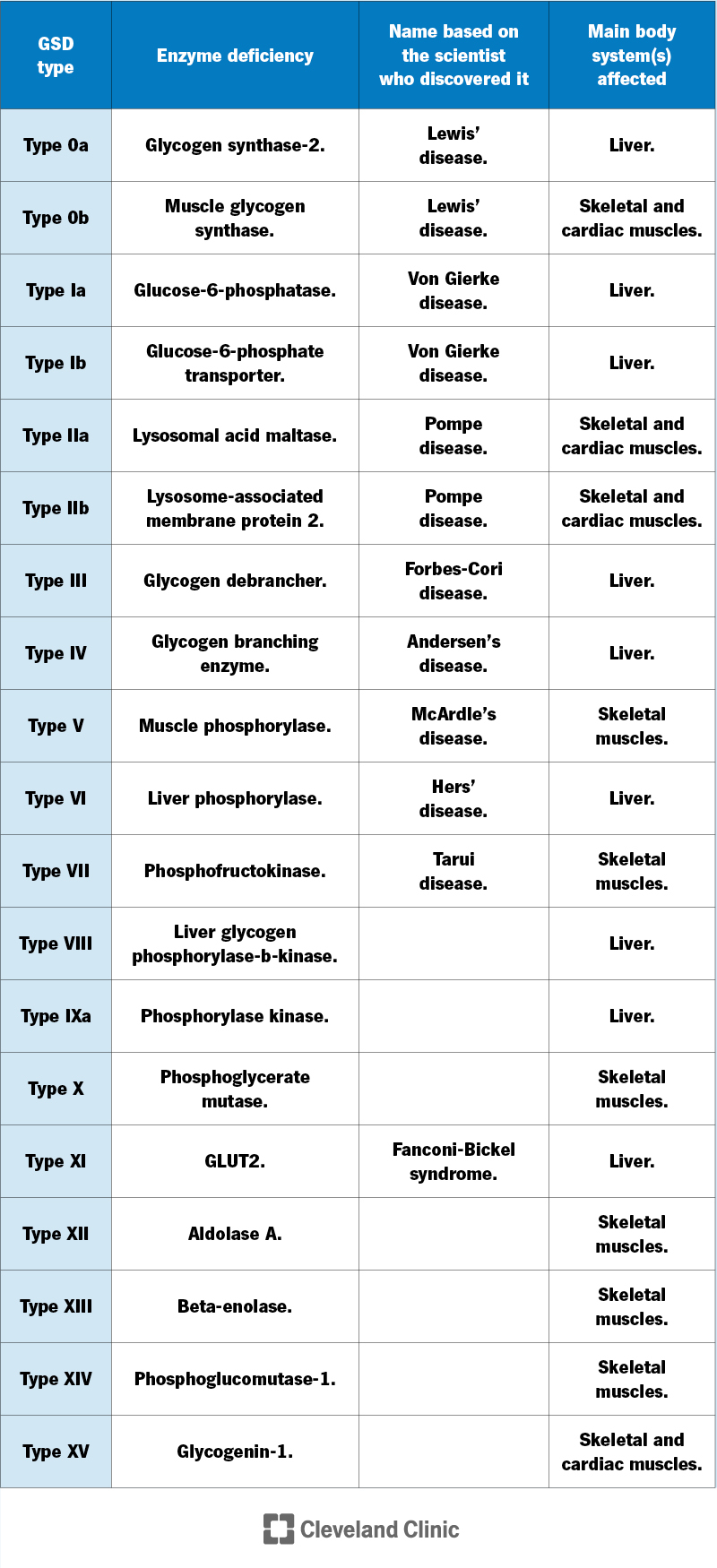
Other Types:
-
GSD IV (Andersen Disease): Branching enzyme deficiency, leading to abnormal glycogen causing liver cirrhosis.
-
GSD VI (Hers Disease): Liver phosphorylase deficiency, milder hepatomegaly and hypoglycemia.
-
GSD IX: Phosphorylase kinase deficiency, often mild, affects liver or muscle.
-
Diagnosis
-
Methods: Enzyme activity assays, genetic testing, liver/muscle biopsy, blood tests (glucose, lactate, lipids, uric acid).
-
Challenges: Overlapping symptoms require specific enzyme or genetic confirmation.
Management
-
Dietary: Frequent feeds, uncooked cornstarch, high-protein diets (for some types).
-
Medical: Enzyme replacement (Type II), allopurinol (for hyperuricemia in Type I), supportive care for complications.
-
Monitoring: Regular checks for hypoglycemia, liver size, kidney function, and muscle damage.
Complications
-
Type-Specific: Liver adenomas/carcinoma (Type I), heart failure (Type II), cirrhosis (Type IV), rhabdomyolysis (Type V).
-
General: Growth failure, osteoporosis, renal dysfunction.
Multiple Choice Questions (MCQs)
For more MCQ Join GPAT TEST SERIES
-
Which enzyme is deficient in von Gierke disease (GSD Type I)?
a) Acid alpha-glucosidase
b) Glucose-6-phosphatase
c) Amylo-1,6-glucosidase
d) Muscle phosphorylase
Answer: b) Glucose-6-phosphatase -
What is a hallmark symptom of Pompe disease (GSD Type II)?
a) Severe hypoglycemia
b) Cardiomyopathy
c) Liver cirrhosis
d) Myoglobinuria
Answer: b) Cardiomyopathy -
Which GSD type is associated with exercise intolerance and muscle cramps?
a) Type I
b) Type III
c) Type V
d) Type IX
Answer: c) Type V -
What is the primary treatment for hypoglycemia in GSD Type I?
a) Enzyme replacement therapy
b) High-protein diet
c) Frequent meals and cornstarch therapy
d) Allopurinol
Answer: c) Frequent meals and cornstarch therapy -
Which GSD type results in the accumulation of abnormal glycogen (limit dextrin)?
a) Type II
b) Type III
c) Type IV
d) Type VI
Answer: b) Type III