Asthma Overview: Definition, Etiology, Symptoms, Diagnosis, Treatment, Prevention and MCQ based on asthma
Notes of Asthma
Asthma: A Detailed Overview
1. Definition of Asthma
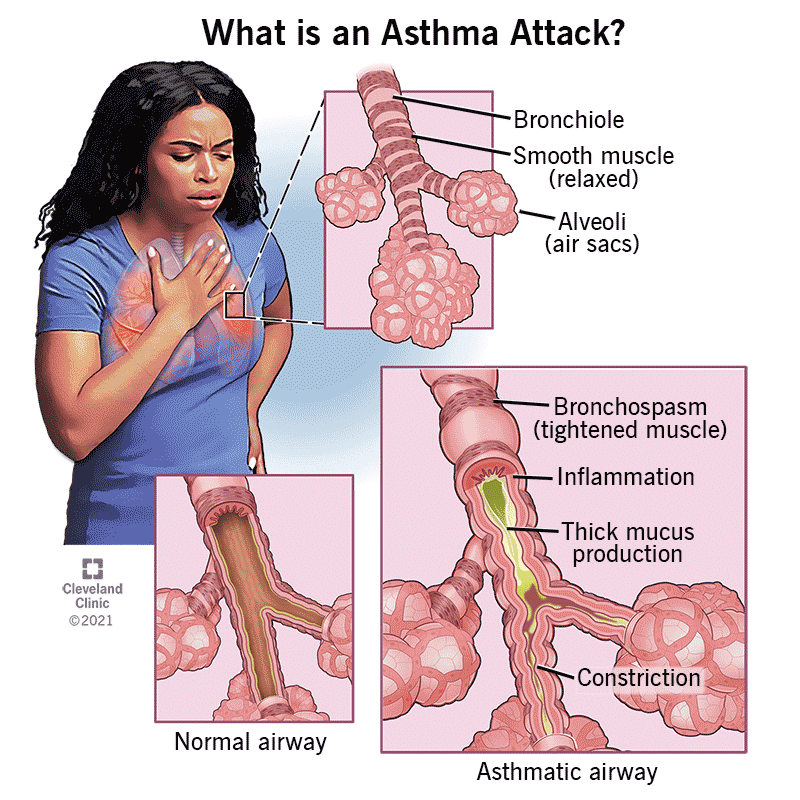
Asthma is a chronic inflammatory disease of the airways in the lungs, characterized by reversible airflow obstruction, bronchial hyperresponsiveness, and airway inflammation. It results in episodes of wheezing, breathlessness, chest tightness, and coughing. These symptoms can vary in frequency and intensity and are often triggered by various environmental or internal factors.
Asthma is typically categorized as an episodic condition, where airway narrowing occurs intermittently but is often reversible either spontaneously or with medication. It affects people of all ages, although it commonly starts in childhood.
Watch below mention video to learn all aspect in easy language
2. Etiology of Asthma
The exact cause of asthma is not fully understood, but it is believed to result from a complex interaction between genetic and environmental factors. The key factors involved in the development of asthma include:
-
Genetic Factors: A family history of asthma, allergic conditions, or other respiratory diseases can increase the risk of developing asthma. Specific genes that influence immune response and lung function are also associated with asthma susceptibility.
-
Environmental Factors: Exposure to allergens (e.g., dust mites, pollen, mold, pet dander), air pollution, cigarette smoke, occupational irritants, and respiratory infections (such as viral infections during childhood) can trigger or worsen asthma. Environmental pollution and climate change also contribute to the rising incidence of asthma.
-
Allergic Reactions: Many cases of asthma are associated with atopic conditions (allergic asthma), where the immune system overreacts to harmless substances (allergens), leading to inflammation of the airways.
-
Airway Hyperresponsiveness: People with asthma have overly sensitive airways that react to stimuli such as cold air, exercise, strong odors, or air pollutants, which leads to bronchoconstriction and inflammation.
-
Respiratory Infections: Infections, particularly in early childhood, can contribute to the development of asthma, particularly viral infections like respiratory syncytial virus (RSV) or rhinovirus.
-
Obesity: Obesity has been linked to asthma, potentially due to the inflammatory state associated with excess body fat and increased respiratory strain.
3. Symptoms of Asthma
Asthma symptoms can vary greatly from person to person and may change over time. Common symptoms include:
- Wheezing: A high-pitched whistling sound when breathing, particularly during exhalation, due to narrowed airways.
- Shortness of Breath: Difficulty in breathing, especially during physical activity or at night.
- Coughing: Persistent coughing, especially at night or early morning, which can be dry or productive.
- Chest Tightness: A sensation of pressure or constriction in the chest, often described as feeling like the chest is being squeezed.
- Increased Mucus Production: Excessive mucus can accumulate in the airways, leading to further airway obstruction.
Symptoms are often triggered by external factors like allergens, cold air, respiratory infections, exercise, smoke, strong odors, or changes in weather.
4. Diagnosis of Asthma
Diagnosis of asthma typically involves a combination of clinical evaluation, medical history, and diagnostic tests. Key aspects include:
-
Medical History: A detailed history is taken to understand the frequency and triggers of symptoms, family history of asthma or allergies, and any potential occupational exposures.
-
Physical Examination: Physical examination may reveal wheezing and signs of respiratory distress, although these may not always be present when the patient is symptom-free.
-
Spirometry (Lung Function Test): The most important diagnostic test for asthma. It measures the volume and speed of air that can be exhaled after taking a deep breath. A reduced Forced Expiratory Volume in 1 second (FEV1) and improvement in FEV1 after using a bronchodilator (a medication that opens up the airways) indicates asthma.
-
Peak Flow Measurement: Measures the maximum speed of exhalation and can help identify variations in airflow during an asthma attack or between attacks. A peak flow meter can be used at home to monitor asthma control.
-
Bronchoprovocation Test (Methacholine Challenge): Used when diagnosis is unclear. Methacholine is a substance that can induce airway narrowing in sensitive individuals, helping to confirm asthma in cases of normal spirometry.
-
Exhaled Nitric Oxide Test: Elevated levels of exhaled nitric oxide can indicate inflammation in the airways, which is common in asthma.
-
Allergy Testing: Skin tests or blood tests to identify specific allergens that may trigger asthma symptoms.
5. Treatment of Asthma
Asthma treatment aims to control symptoms, prevent asthma attacks, and improve overall lung function. Treatment is generally divided into two main categories: long-term control and quick-relief (rescue) medications.
-
Long-Term Control Medications (Preventative):
- Inhaled Corticosteroids (e.g., Fluticasone, Budesonide): The most effective anti-inflammatory treatment. They reduce airway inflammation and prevent symptoms.
- Leukotriene Receptor Antagonists (e.g., Montelukast, Zafirlukast): Used as add-on therapy to reduce inflammation and bronchoconstriction.
- Long-Acting Beta-Agonists (LABAs) (e.g., Salmeterol, Formoterol): Bronchodilators that are used in combination with inhaled corticosteroids to control asthma.
- Mast Cell Stabilizers (e.g., Cromolyn): Prevent the release of histamine and other inflammatory mediators from mast cells.
- Biologic Therapy (e.g., Omalizumab, Mepolizumab): Target specific immune system pathways and are often used for severe asthma not controlled with standard treatments.
-
Quick-Relief (Rescue) Medications:
- Short-Acting Beta-Agonists (SABAs) (e.g., Albuterol, Salbutamol): Provide rapid relief by relaxing bronchial smooth muscle and opening the airways during an acute asthma attack.
- Anticholinergics (e.g., Ipratropium): Often used for acute exacerbations, particularly in combination with SABAs.
-
Oxygen Therapy: In severe asthma attacks, oxygen may be given to maintain adequate oxygen levels in the blood.
-
Oral Corticosteroids: For severe asthma exacerbations, oral corticosteroids (e.g., Prednisone) may be prescribed to reduce inflammation rapidly.
6. Prevention of Asthma
While asthma cannot be cured, there are strategies to prevent asthma symptoms and reduce the frequency of attacks:
-
Avoid Triggers: Identifying and avoiding known triggers (allergens, smoke, cold air, respiratory infections) is key. This may include using air purifiers, avoiding outdoor exercise during high pollen days, or keeping pets out of bedrooms.
-
Regular Medication Use: Adherence to prescribed long-term control medications, even when symptoms are absent, is critical for asthma management.
-
Environmental Control: Reducing exposure to allergens such as dust mites, mold, pet dander, and cockroaches. Use of dust mite-proof pillowcases, bedding, and regular cleaning can help.
-
Vaccinations: Getting annual flu vaccines and ensuring vaccinations against pneumococcus can help reduce the risk of respiratory infections that could exacerbate asthma.
-
Asthma Action Plan: Developing a personalized asthma action plan with the help of a healthcare provider can help patients manage asthma effectively. The plan includes instructions on medication use, recognizing early warning signs of an asthma attack, and knowing when to seek emergency care.
-
Lifestyle Changes: Maintaining a healthy weight, regular physical activity, and managing stress can help reduce asthma symptoms.
-
Allergen Immunotherapy (Allergy Shots): For individuals with allergic asthma, allergy shots may help desensitize the immune system to specific allergens over time.
Conclusion
Asthma is a common and manageable chronic condition that affects the respiratory system. By identifying triggers, adhering to treatment plans, and making lifestyle adjustments, individuals with asthma can lead normal lives with minimal disruption. Early diagnosis and proper management are essential for controlling symptoms and preventing complications. Regular follow-up with healthcare providers ensures that asthma treatment is adjusted as necessary, leading to better quality of life and fewer asthma attacks.
MCQ on Asthma
1. What is the definition of asthma?
a) A chronic infection of the lungs
b) A chronic inflammatory disease of the airways
c) An acute viral infection
d) A condition characterized by excessive mucus production
Answer: b) A chronic inflammatory disease of the airways
2. Which of the following is a major cause of airway inflammation in asthma?
a) Viral infections
b) Allergens
c) Air pollution
d) All of the above
Answer: d) All of the above
3. Which of these factors is most strongly linked to genetic susceptibility to asthma?
a) Viral infections
b) Family history of asthma or allergies
c) Exposure to cigarette smoke
d) Air pollution
Answer: b) Family history of asthma or allergies
4. Asthma symptoms are caused by:
a) Airway constriction
b) Overproduction of mucus
c) Airway inflammation
d) All of the above
Answer: d) All of the above
5. Which of the following is a common symptom of asthma?
a) Headache
b) Wheezing
c) Nausea
d) Joint pain
Answer: b) Wheezing
6. Which of the following is most commonly associated with asthma exacerbation?
a) Eating spicy food
b) Physical activity
c) Exposure to allergens or irritants
d) Eating dairy products
Answer: c) Exposure to allergens or irritants
7. What is the main goal of asthma treatment?
a) To cure asthma
b) To prevent airway inflammation and symptoms
c) To reduce mucus production only
d) To increase airway constriction
Answer: b) To prevent airway inflammation and symptoms
8. What type of medication is used to provide quick relief during an asthma attack?
a) Inhaled corticosteroids
b) Short-acting beta-agonists (SABAs)
c) Leukotriene receptor antagonists
d) Long-acting beta-agonists (LABAs)
Answer: b) Short-acting beta-agonists (SABAs)
9. Which of the following drugs is used for long-term control of asthma?
a) Albuterol
b) Prednisone
c) Fluticasone
d) Ipratropium
Answer: c) Fluticasone
10. Which test is commonly used to diagnose asthma by measuring lung function?
a) Chest X-ray
b) Spirometry
c) Blood test
d) Electrocardiogram (ECG)
Answer: b) Spirometry
11. What does an improvement in FEV1 (Forced Expiratory Volume in 1 second) after bronchodilator use indicate?
a) Asthma is not present
b) The condition is stable
c) The person has an asthma attack
d) Asthma is likely, and the airways are responsive to medication
Answer: d) Asthma is likely, and the airways are responsive to medication
12. What is a characteristic feature of allergic asthma?
a) Bronchoconstriction without inflammation
b) Airway inflammation triggered by allergens
c) Persistent dry cough without wheezing
d) Poor response to inhaled corticosteroids
Answer: b) Airway inflammation triggered by allergens
13. What is the primary mechanism by which inhaled corticosteroids work in asthma treatment?
a) Dilating the airways
b) Reducing inflammation
c) Blocking leukotrienes
d) Inhibiting mucus production
Answer: b) Reducing inflammation
14. Which of the following is a common side effect of long-term use of oral corticosteroids?
a) Weight loss
b) High blood pressure
c) Osteoporosis
d) Increased hair growth
Answer: c) Osteoporosis
15. What is a key feature of asthma prevention?
a) Eliminating all allergens
b) Regular use of long-term control medications
c) Avoiding physical exercise
d) Using only rescue medications during symptoms
Answer: b) Regular use of long-term control medications
16. What class of drug is Montelukast?
a) Leukotriene receptor antagonist
b) Beta-agonist
c) Mast cell stabilizer
d) Corticosteroid
Answer: a) Leukotriene receptor antagonist
17. Which of the following is a biologic therapy used for severe asthma?
a) Omalizumab
b) Prednisone
c) Theophylline
d) Salmeterol
Answer: a) Omalizumab
18. Which of the following is true about asthma attacks?
a) Asthma attacks are caused by viral infections only
b) Asthma attacks are always accompanied by fever
c) Asthma attacks involve acute worsening of symptoms like wheezing and shortness of breath
d) Asthma attacks are not treatable with bronchodilators
Answer: c) Asthma attacks involve acute worsening of symptoms like wheezing and shortness of breath
19. Which of the following tests may be used to confirm airway hyperresponsiveness in asthma?
a) Peak flow measurement
b) Methacholine challenge test
c) Blood oxygen level test
d) Skin allergy test
Answer: b) Methacholine challenge test
20. Which of the following factors is most likely to trigger asthma symptoms in children?
a) Pollen
b) Respiratory infections
c) Physical activity
d) All of the above
Answer: d) All of the above
21. What is the role of leukotriene receptor antagonists in asthma treatment?
a) They dilate the bronchi
b) They prevent the release of histamine
c) They reduce airway inflammation by blocking leukotrienes
d) They improve lung compliance
Answer: c) They reduce airway inflammation by blocking leukotrienes
22. What is the recommended strategy for managing asthma at home?
a) Only use medications when symptoms are severe
b) Regular monitoring with a peak flow meter and adherence to an asthma action plan
c) Never use inhaled corticosteroids
d) Avoid physical exercise
Answer: b) Regular monitoring with a peak flow meter and adherence to an asthma action plan
23. Which of the following medications can be used as both a long-term controller and a quick-relief medication in asthma?
a) Fluticasone
b) Budesonide
c) Salmeterol
d) Budesonide/Formoterol combination
Answer: d) Budesonide/Formoterol combination
24. Which environmental factor is most commonly associated with worsening asthma symptoms?
a) Humid environments
b) Cigarette smoke
c) Fresh air
d) High altitudes
Answer: b) Cigarette smoke
25. Which of the following is NOT a recommended preventive measure for asthma?
a) Allergen avoidance
b) Regular exercise
c) Long-term medication adherence
d) Avoiding any form of physical activity
Answer: d) Avoiding any form of physical activity