Pathophysiology of Asthma : Simplified, MCQ on Pathophysiology of Asthmatic attack
Notes for Students
Pathophysiology of Asthma
Asthma is a chronic inflammatory disease of the airways that leads to variable airflow obstruction, bronchial hyperresponsiveness, and airway remodeling. It primarily affects the bronchi (large and small airways), leading to inflammation, smooth muscle constriction, and mucus production. This inflammation results in intermittent symptoms such as wheezing, shortness of breath, chest tightness, and coughing, particularly in response to triggers such as allergens, irritants, or respiratory infections.
The pathophysiology of asthma can be broken down into several stages: airway inflammation, bronchoconstriction, increased mucus production, and airway remodeling.
1. Airway Inflammation
The hallmark of asthma is airway inflammation. This inflammation is primarily triggered by environmental factors such as allergens (pollen, dust mites, pet dander), irritants (smoke, pollution), or viral infections. The process begins when an allergen or irritant is inhaled, activating the immune system. Here’s how:
-
Dendritic Cells in the airway epithelium capture allergens and present them to T-helper cells (TH2 cells), which are involved in allergic responses.
-
Activation of T-helper Cells (TH2): In asthmatic patients, TH2 cells are the predominant immune response. They release a variety of cytokines, including IL-4, IL-5, and IL-13.
- IL-4 and IL-13 promote IgE production by B-cells. IgE antibodies bind to mast cells, which become sensitized to the specific allergen.
- IL-5 is crucial for the activation and recruitment of eosinophils, which are inflammatory cells that play a central role in asthma inflammation.
-
Mast Cells and Eosinophils: Upon re-exposure to the allergen, mast cells release histamine, leukotrienes, prostaglandins, and cytokines, which lead to immediate bronchoconstriction and further recruitment of eosinophils and neutrophils.
- Eosinophils release toxic proteins such as major basic protein that damage airway epithelial cells, perpetuating inflammation.
- The release of cytokines and other inflammatory mediators further increases airway inflammation and contributes to long-term damage.
Watch below mention video to learn all aspect of asthma pathophysiology in easy manner
2. Bronchoconstriction
The inflammation in asthma leads to the contraction of the smooth muscle surrounding the airways, resulting in bronchoconstriction. This is the most immediate physiological response to inflammation and can cause severe symptoms during an asthma attack.
- Bronchial Smooth Muscle Constriction: The release of leukotrienes (e.g., LTD4) and prostaglandins causes bronchoconstriction by acting on the smooth muscle.
- Neural Mechanisms: The vagus nerve also plays a role in bronchoconstriction via the release of acetylcholine, which binds to muscarinic receptors on airway smooth muscle, promoting constriction.
The airway narrowing caused by bronchoconstriction leads to difficulty in exhaling air from the lungs, resulting in the hallmark wheezing and shortness of breath seen in asthma.
3. Increased Mucus Production
In asthma, inflammation of the airway lining results in increased mucus production from goblet cells and submucosal glands. This thick, viscous mucus further obstructs the already narrowed airways, worsening airflow limitation.
- Mucus Hypersecretion: Cytokines and eosinophils promote the excessive production of mucus in the airways, contributing to the airway obstruction.
- The mucus plugs formed in the airways can further exacerbate the airflow limitation, leading to chronic symptoms and increased susceptibility to infections.
4. Airway Remodeling
Prolonged inflammation in asthma can lead to airway remodeling, which is characterized by structural changes in the airways that result from chronic inflammation. These changes make the airways more responsive and less able to return to normal after an asthma attack.
- Increased Smooth Muscle Mass: There is an increase in the smooth muscle mass of the airways, leading to a greater potential for bronchoconstriction.
- Fibrosis: Chronic inflammation can lead to the deposition of collagen and other extracellular matrix components in the airway walls, resulting in fibrosis. This makes the airways stiffer and less able to dilate.
- Mucous Gland Hyperplasia: There is an increase in the number and size of goblet cells and mucous glands, contributing to increased mucus production.
- Thickening of the Basement Membrane: The basement membrane of the airway epithelium becomes thickened due to collagen deposition, contributing to long-term airway narrowing and reduced lung function.
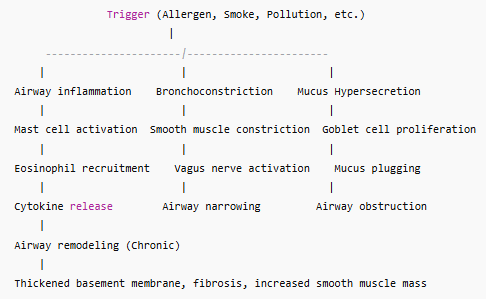
Diagram of Asthma Pathophysiology
Here’s a simplified diagram representing the key processes involved in asthma pathophysiology:
Summary
The pathophysiology of asthma involves a complex interplay of immune responses, airway inflammation, and structural changes in the airways. Key events include:
- Airway inflammation due to the activation of immune cells like mast cells, eosinophils, and T-helper cells.
- Bronchoconstriction caused by the contraction of smooth muscles in the airway.
- Increased mucus production that obstructs airflow.
- Airway remodeling in chronic asthma, which leads to permanent changes in the airway structure and function.
Effective asthma management focuses on controlling airway inflammation, preventing bronchoconstriction, and minimizing exposure to triggers.
MCQ on Asthma Pathophysiology
1. Which of the following is the primary cause of airway inflammation in asthma?
a) Bacterial infections
b) Immune response to allergens
c) Increased airway mucus production
d) Decreased air pollution
Answer: b) Immune response to allergens
2. What is the role of T-helper 2 (TH2) cells in asthma?
a) They release cytokines that promote airway inflammation and IgE production
b) They directly cause bronchoconstriction
c) They inhibit mast cell degranulation
d) They increase mucus production in the lungs
Answer: a) They release cytokines that promote airway inflammation and IgE production
3. Which cell type is primarily involved in the chronic inflammation seen in asthma?
a) Neutrophils
b) Eosinophils
c) Macrophages
d) Lymphocytes
Answer: b) Eosinophils
4. What is the primary mediator responsible for bronchoconstriction in asthma?
a) Histamine
b) Leukotrienes
c) Prostaglandins
d) Interleukins
Answer: b) Leukotrienes
5. The release of which substance from mast cells contributes to early-phase bronchoconstriction in asthma?
a) Histamine
b) IgE
c) Nitric oxide
d) Interleukin-5 (IL-5)
Answer: a) Histamine
6. Which of the following is a key characteristic of airway remodeling in asthma?
a) Decreased number of goblet cells
b) Thickening of the airway basement membrane
c) Reduction in airway smooth muscle mass
d) Increased airway lumen diameter
Answer: b) Thickening of the airway basement membrane
7. What effect does eosinophil activation have in the airways of asthma patients?
a) It causes a reduction in airway smooth muscle contraction
b) It releases toxic proteins that damage the airway epithelium
c) It prevents mucus production
d) It reduces airway inflammation
Answer: b) It releases toxic proteins that damage the airway epithelium
8. Which of the following processes is responsible for the increased mucus production in asthma?
a) Decreased goblet cell proliferation
b) Decreased inflammation in the airway
c) Increased proliferation of goblet cells and mucous glands
d) Decreased blood flow to the airway epithelium
Answer: c) Increased proliferation of goblet cells and mucous glands
9. What is the effect of airway smooth muscle hypertrophy in asthma?
a) It leads to airway dilation
b) It causes long-term airway narrowing and bronchoconstriction
c) It prevents mucus production
d) It reduces airway inflammation
Answer: b) It causes long-term airway narrowing and bronchoconstriction
10. Which of the following is a key feature of the late-phase response in asthma?
a) Immediate bronchoconstriction and wheezing
b) Airway inflammation and recruitment of inflammatory cells like eosinophils
c) Immediate relief after using bronchodilators
d) A decrease in airway remodeling
Answer: b) Airway inflammation and recruitment of inflammatory cells like eosinophils